Types of Shoulder Instability: Symptoms, Diagnosis & Treatment Options
The shoulder is the most flexible joint in the body, allowing for full rotation and a great range of motion. This mobility, however, leaves the shoulder highly susceptible to injury and resulting instability.
Approximately 1% to 2% of people will suffer a shoulder dislocation in their lifetime and young athletes are at a particularly high risk of shoulder instability events – 95% of which occur in the anterior direction.
When a shoulder dislocates, it becomes more vulnerable to future dislocations. In addition to dislocations, other conditions – such as subluxation and hyperlaxity – can lead to shoulder instability.
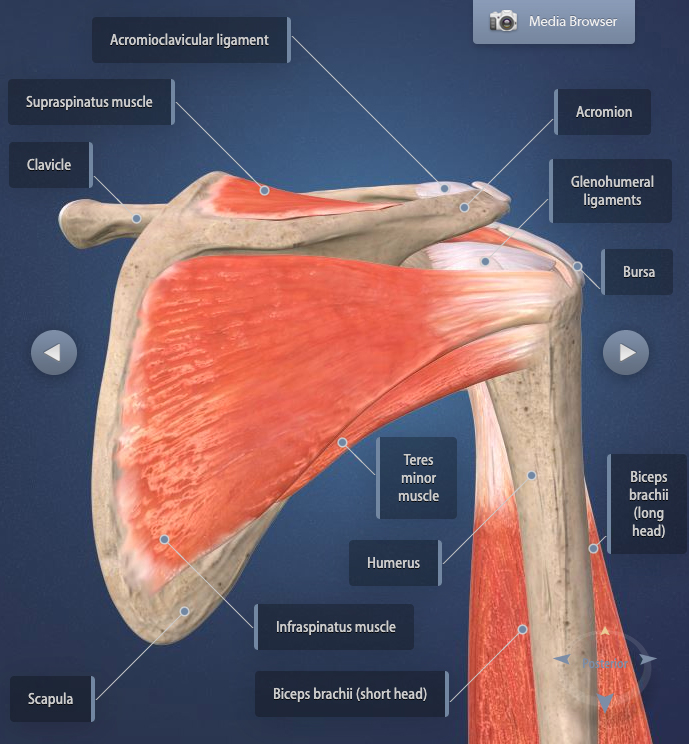
Shoulder Anatomy
The shoulder is a complex joint of four smaller joints made up of three bones (humerus, scapula and clavicle), connective tissue (ligament system called the shoulder capsule), muscles, tendons, nerves and blood vessels. In the glenohumeral joint of the shoulder, the head of the humerus (upper arm) fits into a shallow socket in the shoulder blade called the glenoid.
The shoulder capsule works to keep the head of the humerus in the center of the glenoid socket and attaches the upper part of the humerus to the scapula (shoulder blade). In this ball-and-socket joint, the ball (head) of the humerus is three to four times bigger than the glenoid socket. While this allows for greater movement of the shoulder joint, it also leaves the glenohumeral joint prone to dislocation.
The labrum, rotator cuff and other muscles and tendons in the shoulder joint also work to stabilize the joint. Dislocations, labrum tears, rotator cuff tears and other shoulder injuries can all lead to chronic shoulder instability.
Types of Shoulder Instability
There are three general types of shoulder instability.
Anterior Shoulder Instability
The most common type of shoulder instability, anterior shoulder instability, typically occurs when the shoulder is in abduction and external rotation. Abduction is when you raise your arm laterally away from your body (think making a “T” with your arms) and external rotation is when you rotate your elbows forward. A good example of a shoulder in abduction and external rotation is when you throw a ball.
Posterior Shoulder Instability
Posterior instability is much less common than anterior instability and typically stems from muscle contractions (versus trauma in athletes) like those from seizures or severe electric shock. In a posterior dislocation, the head of the humerus is dislocated from the posterior labrum and the glenoid socket.

Multidirectional Shoulder Instability
Unlike anterior and posterior shoulder instability, multidirectional shoulder instability is not a result of dislocation or injury. This type of instability is caused by a congenital hyperlaxity of the glenohumeral joint capsule (naturally looser ligaments in the shoulder) or laxity as a result of repetitive overhead motions (from sports, occupations, etc.).
Someone with congenital hyperlaxity or developed laxity is particularly susceptible to chronic multidirectional instability after a rotator cuff injury or tear.
Symptoms
The three different types of shoulder instabilities have a variety of symptoms; consult an orthopedic shoulder specialist for an accurate diagnosis of your symptoms.
Shoulder instability symptoms include:
- Hearing or feeling a “pop” in the shoulder
- Significant pain and discomfort
- Inability to move the shoulder or feel that the shoulder is “stuck”
- Feeling of increased movement in the glenoid socket
- Difficulty lifting the arm overhead
- Weakness in the shoulder and/or arm
Chronic Symptoms Include:
- Repeated instances of the shoulder “giving out” or getting “stuck”
- Repeated shoulder dislocations
- Ongoing sensation of the shoulder slipping in and out of the glenoid socket or feeling loose
- Feeling like the shoulder is “dead” or just hanging there
Diagnosis

There are a number of tests your orthopedic shoulder surgeon will conduct to diagnose shoulder instability, including the load-and-shift maneuver, the relocation test, the drawer test, the sulcus test and the anterior apprehension test.
During these tests, your doctor will manipulate your joint and ask you to move your arm and shoulder in specific ways to evaluate your shoulder injury. If necessary, your orthopedic specialist will order X-rays to look for any bone injuries in your joint or an MRI to see if you have any additional ligament or tendon damage.
Treatment Options
Closed Reduction
If you suffer from an anterior or posterior shoulder dislocation, your orthopedic surgeon will start with a closed reduction. This procedure involves manually setting the shoulder joint back into its proper position. When successful, severe pain typically subsides almost immediately. However, if the closed reduction fails, surgery may become necessary to properly stabilize the joint.
Surgery
If you experience recurring shoulder dislocations, weakness, or torn ligaments, surgery may be required. In rare cases, surgery becomes essential when nerve or blood vessel damage occurs within the shoulder joint. Seeking treatment early can help restore function and prevent further complications.
Immobilization
Immobilizing your shoulder joint may be necessary. This applies whether your shoulder injury requires a closed reduction, surgery, or no procedure at all. Keeping the joint in place helps ensure proper healing and prevents further injury.
Physical Therapy Exercises
Your doctor may prescribe physical therapy to help strengthen your shoulder muscles to improve stability in and around the joint. Your physical therapist will often provide a program of shoulder instability exercises for you to do at home, as well.
If you’re suffering from shoulder instability or have experienced a dislocation, please see an orthopedic specialist for treatment. If you have any questions about shoulder instability, symptoms or treatments, please contact us or leave a comment below.
1 Comment
Permalink
Reviewing your diagram and details above, it feels like Anterior Shoulder Instability, an abduction in my left shoulder. After seeing DMC, I did get an MRI but no explanation or understanding in the RAD read; seemingly a lot going on!
I was a patient of Dr. Heiden’s many years ago with a torn bicept tendon operated on the right shoulder.
++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++