What Is Osteoarthritis?
Osteoarthritis is the most common form of arthritis, in which affected joints exhibit pain, stiffness, and decreased flexibility. The condition can be caused by many factors, including joint injury and overuse alongside advancing age. Since osteoarthritis can’t be reversed, preventing it is key to living your most mobile life.
Osteoarthritis Symptoms
According to the Centers for Disease Control (CDC), osteoarthritis affects 32.5 million adults in the United States. It typically comes on slowly and gets worse with age.
Joints affected by osteoarthritis often exhibit:

- Tenderness, aching, and pain
- Stiffness, loss of flexibility, and decreased range of motion
- Swelling
- A catching or grating sensation during movement
- A feeling of instability in the joint, whether shoulder instability, knee instability, or patellar instability
Osteoarthritis (OA), also called degenerative joint disease, typically gets worse with time and can result in chronic pain. It can make joints so stiff that normal tasks become difficult, and the pain and disruption can also impact mental health.
Treating injuries to cartilage and the subsequent development of osteoarthritis is challenging, so it’s important to see a doctor who specializes in orthopedic joint care. Your specialist will discuss your symptoms, perform a physical exam, and take diagnostic images like an X-ray or MRI. Diagnostic images allow your orthopedic specialist to evaluate the severity of your OA and its impacts on your tissues.
What causes OA?
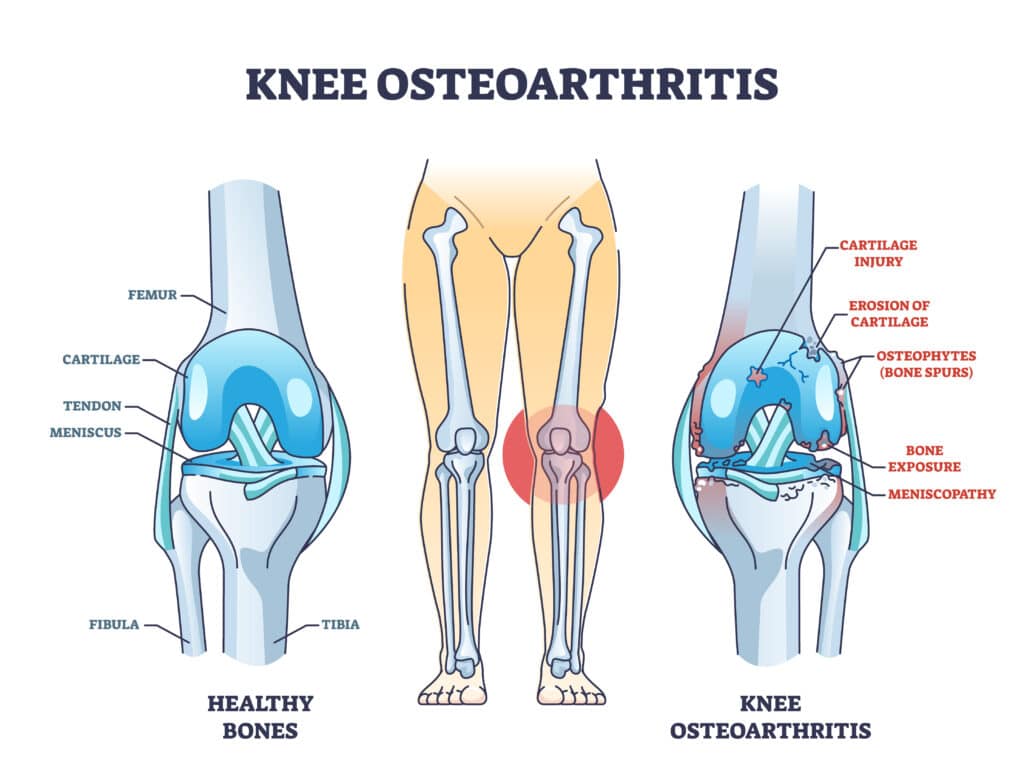
The ends of your bones have a protective layer of slippery cartilage called articular cartilage that acts as a shock absorber for your joints. Articular cartilage is tough and flexible, but it can be damaged. Cartilage damage is often caused by injury or overuse and can result in deterioration, leading to OA.
Because there’s no blood supply going to articular cartilage, it has a very limited ability to repair itself. Thus, as cartilage issues progress and OA develops, bone can rub against bone, changing the structure of the entire joint. Over time, this rubbing can deteriorate the bone or cause a bone spur to form, and attached connective tissues can also break down. The joint lining can become swollen and inflamed.
Certain segments of the population are more likely to develop osteoarthritis, including:
- Those with joint injuries, such as sports injuries or traumatic injuries
- Those with repeated joint stress, which can be caused by activities like running
- Women
- People over the age of 50
- Overweight and obese individuals
- Those with a family history of OA
- People with bone alignment issues or certain metabolic diseases
Osteoarthritis can affect virtually any joint in the body, but because the knee is a weight-bearing joint prone to injury, knee osteoarthritis is very common. For this same reason, OA also tends to affect the hips and feet. Osteoarthritis in the hands often runs in families, and people can also get OA in their lower back and necks.
Osteoarthritis Treatment
While there is no cure for OA, there are things you can do to treat its symptoms. Use these osteoarthritis self-care treatments under the guidance of your orthopedic specialist to ensure you don’t exacerbate your symptoms.
- RICE: Rest, ice 20 to 30 minutes at a time, and compress and elevate the joint
- Increase overall activity levels
- Perform physical therapy exercises as directed
- Improve muscular strength
- Lose weight, if necessary
- Take over-the-counter pain relievers or prescription medications as directed
- Use an unloader brace, canes, or crutches to lessen the weight on the affected joint
- Ask about corticosteroid or hyaluronic acid injections
Surgery for OA
Cartilage does not heal well on its own, so conservative treatment approaches may not be sufficient in certain cases. Surgery will be the best option for some people with osteoarthritis to live as desired.
In arthroscopy, your surgeon uses small instruments inserted through small incisions to see inside your joint and make repairs. If performing an osteotomy, your surgeon will remove or add a wedge of bone to the damaged joint to realign it and remove pressure. If you need arthroplasty or total joint replacement, part or all of your damaged joint will be removed and replaced with a prosthetic joint.
Osteoarthritis vs Rheumatoid Arthritis
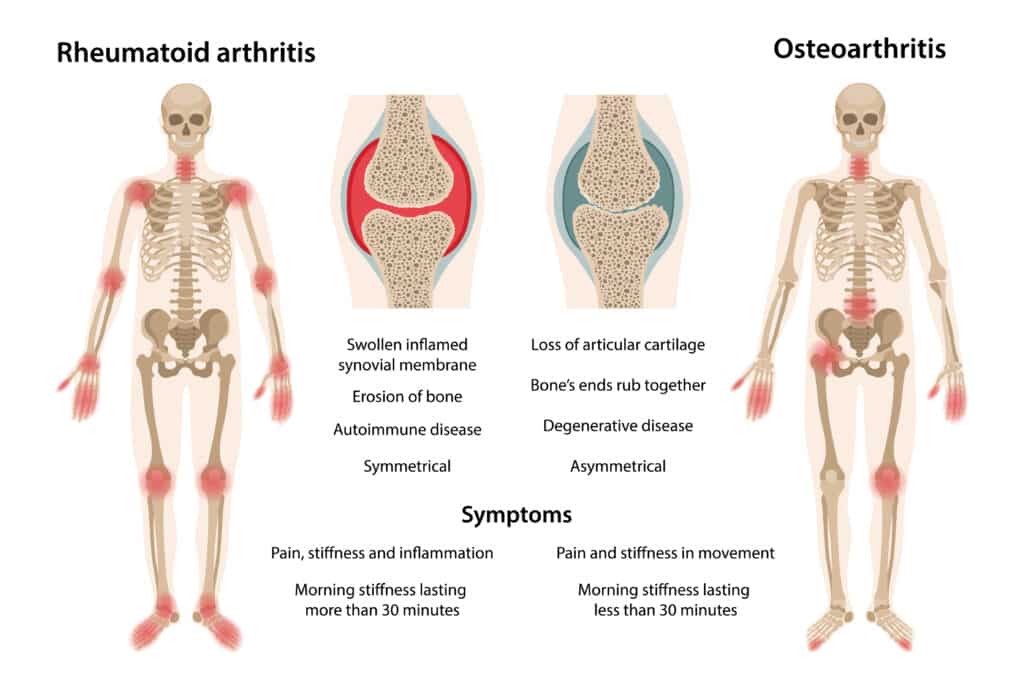
The main difference between osteoarthritis and rheumatoid arthritis (RA) is that OA is caused by joint cartilage breaking down due to things like injury and overuse, whereas RA is an autoimmune disease that causes the immune system to attack the body’s joints.
RA often affects the hands and feet, generally comes on relatively quickly, and is typically symmetrical, with the same joints on both sides of the body feeling symptoms. OA tends to begin in a single joint or be more noticeable on one side of the body than the other. Because RA is an autoimmune issue, you may have recurring feelings of being generally ill, whereas OA causes no whole-body symptoms. If you live in an area with ticks, you will also want to be aware of the potential of developing Lyme arthritis after Lyme disease.
Please contact us or comment below if you have questions about osteoarthritis symptoms or prevention and would like to speak with an orthopedic specialist.
1 Comment
Permalink
I am in stage 2 of OA how to take precautions my self