Hip Osteoarthritis
“I don’t bounce back like I used to.” Have you heard yourself say a version of this yet? As we age, previous injuries and wear and tear plague us in new ways. Hips, knees, and backs get achy — sometimes after a favorite athletic activity and sometimes because we’ve been too sedentary.
Osteoarthritis (OA) is one such condition that impacts aging individuals. Eighty-eight percent of people with OA are 45 years of age or older.
Osteoarthritis can affect any joint, but it’s most common in weight-bearing joints like the knees, hips, and spine. OA’s characteristic pain and stiffness tend to worsen over time. Since there’s no cure, early diagnosis and symptom management are integral for maintaining healthy joint function.
Hip Anatomy and Arthritis
The word arthritis means inflammation of a joint. There are hundreds of types of arthritis, but osteoarthritis, aka wear-and-tear arthritis, is the most common.
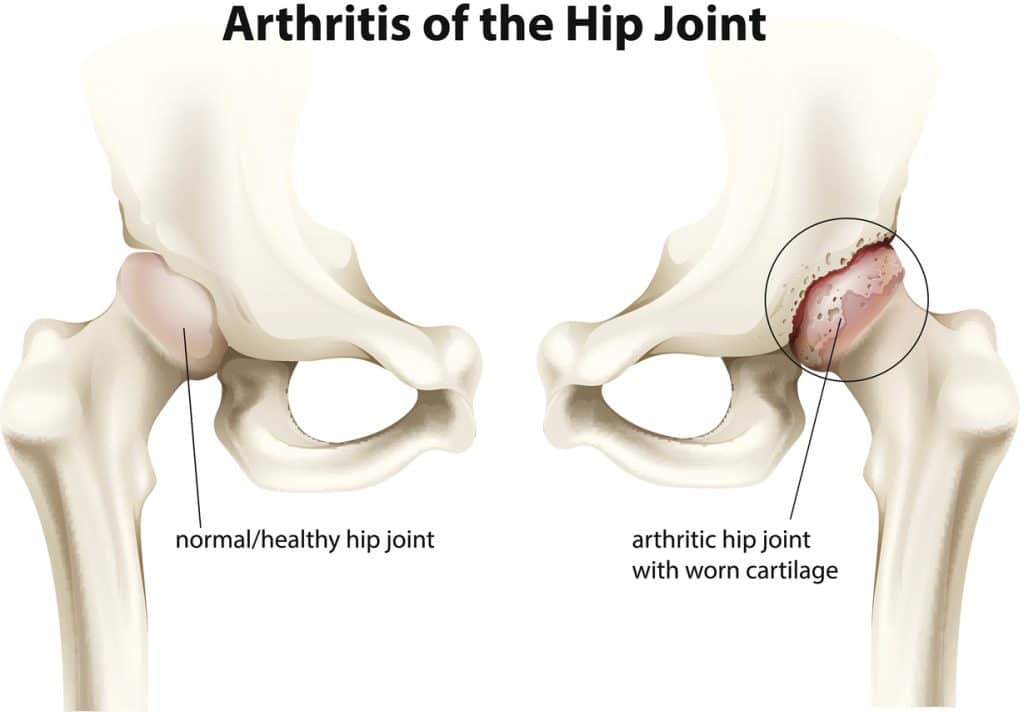
The hip joint is the body’s largest ball and socket joint — the type of joint capable of the most mobility. The ball of this joint is the round head of the femur, and it fits into a cup-shaped socket in the pelvis called the acetabulum.
The femur and acetabulum are covered with articular cartilage. This smooth, slippery, rubbery substance protects and cushions the bones as they move. It changes shape when it’s compressed, acting as a shock absorber under impact.
Our bodies do not grow new cartilage if injured, though it can do some self-repair when damaged. Cartilage can gradually wear away with time, becoming frayed and rough. The cartilaginous space between the femur and acetabulum gets smaller as this happens.
In advancing osteoarthritis, the two bones eventually begin to rub against each other. This damages the bones and can cause bone spurs (osteophytes). The entire joint, including its lining (synovium) and connective tissue, becomes inflamed.
What causes osteoarthritis?
While OA generally affects those advancing into their 40s, 50s, and above, increasing age is not the only cause. Other contributing factors include:
- Female gender
- Those with osteoarthritis in their family history
- Previous hip joint injuries
- Being overweight or obese
- Developmental hip issues like hip dysplasia
Interestingly, you can still develop OA without having any of these risk factors.
Hip Osteoarthritis Symptoms

Two of the main symptoms of hip osteoarthritis are hip pain and stiffness. These symptoms impact your ability to participate in your favorite sport and activities.
They also impact the small moments that make up daily life. With advancing hip osteoarthritis, routine tasks like putting on shoes, climbing stairs, and getting into and out of cars can become painful.
The most common symptoms of hip osteoarthritis are:
- Pain, which can be dull and achy or sharp, is generally felt in the hip, groin, thigh, buttocks, or knee, and may worsen with rainy weather
- Stiffness that makes it hard to walk or bend
- Loss of flexibility and range of motion
- Limping
- A locking, sticking, or grating sensation
- The sound of crunching or grinding
- Tenderness
- Swelling
While arthritis pain and stiffness are typically worse first thing in the morning or after sitting for an extended period, they become more constant over time. Sleeping can become difficult. The combination of pain, disruption of activities, and loss of sleep increase the chance of depression for OA sufferers.
Although most with OA develop symptoms over time, sudden onset is possible. See your orthopedic hip specialist if you have any of these symptoms. They’ll help you slow the progression of the deterioration and improve your hip’s function.

Diagnosing Hip Osteoarthritis
Diagnosing hip OA can be challenging at first because symptoms typically develop slowly over time, and the pain can appear in different locations (such as the thigh or buttocks).
Your orthopedic hip specialist will perform a physical exam and take diagnostic images using an X-ray, MRI, or CT scan. Imaging shows the degree to which the joint space has narrowed and whether bone spurs have begun to form.
There’s no cure for OA. Early diagnosis and management help manage pain so you can stay active.
Treating Hip Osteoarthritis
The treatment goals of hip osteoarthritis are decreasing pain and increasing mobility. Both nonsurgical and surgical methods can improve the hip’s function.
Nonsurgical methods center around lifestyle modifications and pain management. They include:

- Minimizing activities that exacerbate your symptoms, such as climbing stairs
- Increasing the proportion of low-impact activities like swimming or cycling vs. high-impact activities like running or tennis
- If necessary, losing weight to reduce the stress put upon the hip
- Exercises for flexibility, range of motion, and strengthening hip and leg muscles
- Supporting your mobility with a cane, crutches, or a walker
- Helping manage pain by using a long-handled reacher to retrieve items from the floor or high places
- Trying hot packs, cold packs, and pain-relieving creams as directed
- Talking with your specialist about non-steroidal anti-inflammatory medications and oral or injected corticosteroids to help relieve pain
For cases of hip OA that are not aided by nonsurgical methods and are causing a significant disruption to your daily life, surgical options are available. The most common hip osteoarthritis surgeries include:
- Total hip replacement — The surgeon removes both the damaged acetabulum and femoral head. They use new metal, plastic, or ceramic surfaces on both bones to restore hip function. Hip replacement recovery time is lessening with new surgical developments.
- Hip resurfacing — The damaged bone of the acetabulum is removed and replaced with metal. The head of the femur is not removed, instead, it’s capped with a smooth metal covering.
- Osteotomy — This procedure is only rarely used in relieving the symptoms of hip OA. It consists of cutting and realigning the head of the femur or the acetabulum to take pressure off the hip joint.
Post-surgery, you’ll need the help of a cane, crutches, or a walker while you heal. Performing physical therapy exercises will help you regain your strength and range of motion.
Final Thoughts
Preventing hip osteoarthritis is the most effective and efficient way to avoid lifelong symptoms. Exercise regularly to keep your muscles and joints strong and to maintain a healthy weight.
Please contact us for more ways to decrease your risk of hip osteoarthritis or if you have symptoms you’d like to discuss with an orthopedic hip specialist.
Leave a Reply